As we learn about bacteria and viruses pathogenic to humans, it is also important to consider the human microbiome. Studies are beginning to reveal connections between these communities of microorganisms inside our bodies and both human health and disease. The microbiome role in human disease was first introduced to me in Microbiology on the first day of class, where Dr. Cramer discussed a study linking the bacteria Porphyromonas gingivalis to citrullination of proteins, and possibly autoimmune diseases. P. gingivalis, is just a single microorganism though, and when you study the human microbiome, it is important to consider the interactions between the many different organisms that it consists of. Based on the number of studies that I came across in my research, I believe that there is a great deal we can learn about the human body from studying the microbiomes, even possible treatment and prevention methods for some very serious diseases.
Keeping with the Alzheimer’s link, there are several groups studying exactly how the microbiome may be involved in neurodegenerative diseases like Alzheimer’s, Parkinson’s, and Huntington’s. A study conducted by scientists at the University of Chicago showed some evidence that gut microbiota can actually worsen the progression of diseases like Alzheimer’s. The study used transgenic mice with genetic predispositions to beta-amyloid proteins and monitored inflammation causing microglia that are linked to cell death in neurodegenerative diseases in relation to gut microbiota. When these mice were given antibiotics, they showed fewer beta-amyloid plaques and more healthy microglia (as opposed to the inflammation-causing microglia) (Sternberg, n.p.). When a fecal transplant from healthy mice that had not been treated with antibiotics was done, the mice showed more beta-amyloid plaques and elevated markers for the inflammation-causing microglia. Although this observation was only made in male mice, this study still provides a hint into the potential direct or even indirect role that our microbiome plays on human diseases.
Most studies are aimed at discovering the mechanism behind our microbiomes influence on the immune system, whether it is the microorganisms themselves or their metabolites (Bender, n.p.). One theory called “molecular mimicry” chops their role down to host microbiome genes that share similarities with our own genes. Basically, when attacking the microbiota, our body gets confused and attacks similar self-proteins as well (Bender, n.p.). This specific mechanism is thought to be related to the development of both lupus and rheumatoid arthritis. But enough talk about how microbiota contribute to disease, how can we use this information for therapies against autoimmune diseases? The basis of using microbiota as treatment is that some bacteria are anti-inflammatory, while others are proinflammatory (and disease causing). So, using fecal transplants and probiotics to promote the anti-inflammatory types could provide significant relief for those suffering from autoimmune diseases. As more research is being conducted, scientists are considering the possibility of using these therapies as treatment for some diseases, as well as changes in diet to promote the growth of “healthy” microbiota.
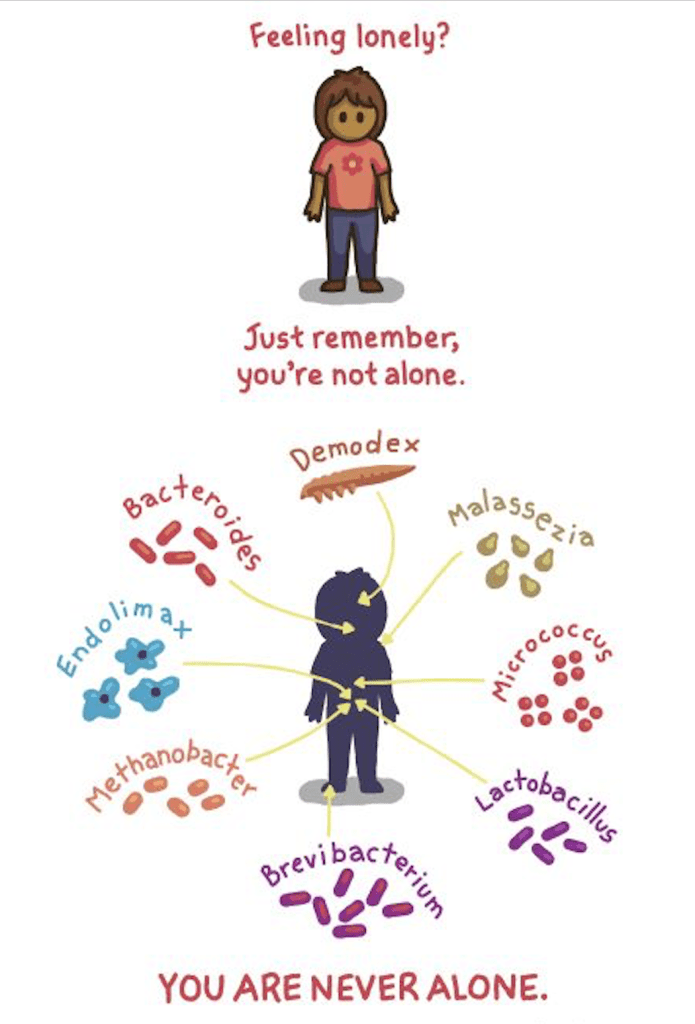
Frankly, the idea that bacteria in our guts can have an effect on our bodies outside of digestion is fascinating. Our mood, weight, and health, among other things are all influenced by the types of microorganisms colonizing us, so remember that when you’re living on a diet of just Starbucks and Chick-fil-A.