With the COVID-19 pandemic going on, it is hard to focus on other threats to public health, but there are still ongoing pandemics that we cannot ignore. Tuberculosis (TB) is one that I want to focus on for this post. With a quarter of the world suffering from TB infections, it remains the world’s top infectious killer (WHO). For this reason, the World Health Organization has been taking steps towards eliminating TB by 2030. Just recently at the 2020 World TB day conference, WHO emphasized their efforts to provide preventative care around the world. The targets for these increased measures are those who are most at-risk for the infection, including those with HIV, family members of individuals with TB, and people living in crowded communities (WHO). Based on what we know about TB (and COVID-19), controlling the spread of a pandemic is the key to eliminating it.
The biggest distinction between COVID-19 and TB is the type of pandemic that they are. COVID-19 is a new pandemic that has spread rapidly, whereas TB is a slow pandemic that has been around for quite some time. The individuals that are affected also differ, with children being an at-risk group for TB. In 2018, 1.1 million children suffered from TB, of which 200,000 died (Wingfield, p.1). Amidst the COVID-19 crisis, though, it is also important to evaluate how the two interact, as the new pandemic can change the way TB affects some populations (Wingfield, p.1). It is possible that COVID-19 could increase or decreased TB transmission. COVID-19 is overwhelming the nation’s healthcare system, so it could be possible that some people are not receiving treatment for TB as a result. I say all this to emphasize the epidemiological standpoint of the two pandemics, which changes a lot about each.
Now, as we look at TB from a microbiology standpoint, there is still a lot of things that scientists don’t know about Mycobacterium tuberculosis, which is the bacteria that causes TB. There are several studies aimed at learning more about the bacterium, and one at Stanford Linear Accelerator Center (SLAC) has discovered a transport protein in its membrane that may play a role in the disease. The protein was shown to have a “huge interior pocket,” which could allow large molecules to enter the bacterial cell (Collins, n.p.) This particular protein is of interest because the bacteria’s vitamin B12 uptake has been shown to play a vital role in its survival and progression into TB disease (Collins, n.p.) Although it is a new finding, the researchers at SLAC have still found a potentially critical piece to the puzzle that is TB. Future research needs to be conducted to figure out if vitamin B12 is transported using this new protein, but it is still progress being made in favor of developing new treatments and better understanding the bacterium.
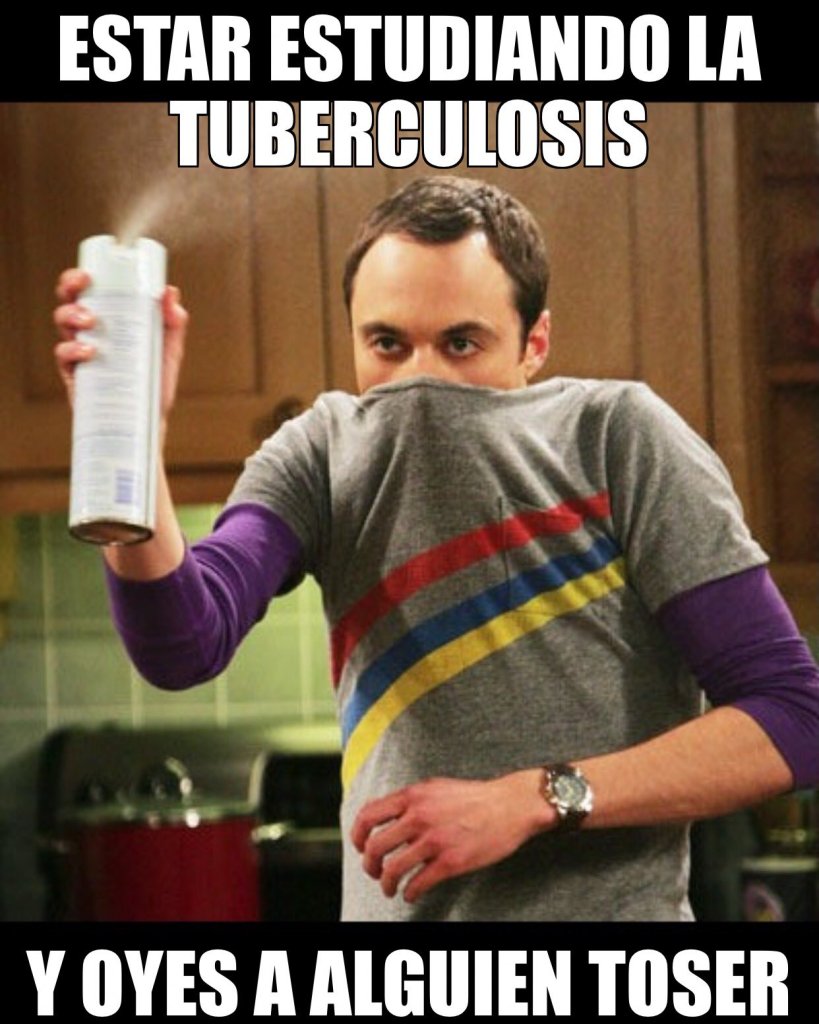
The meme for today is in Spanish, but it reads: “when you’re learning about tuberculosis and you hear someone cough.”